Health insurance: Disparities in Billing and Claims Processing
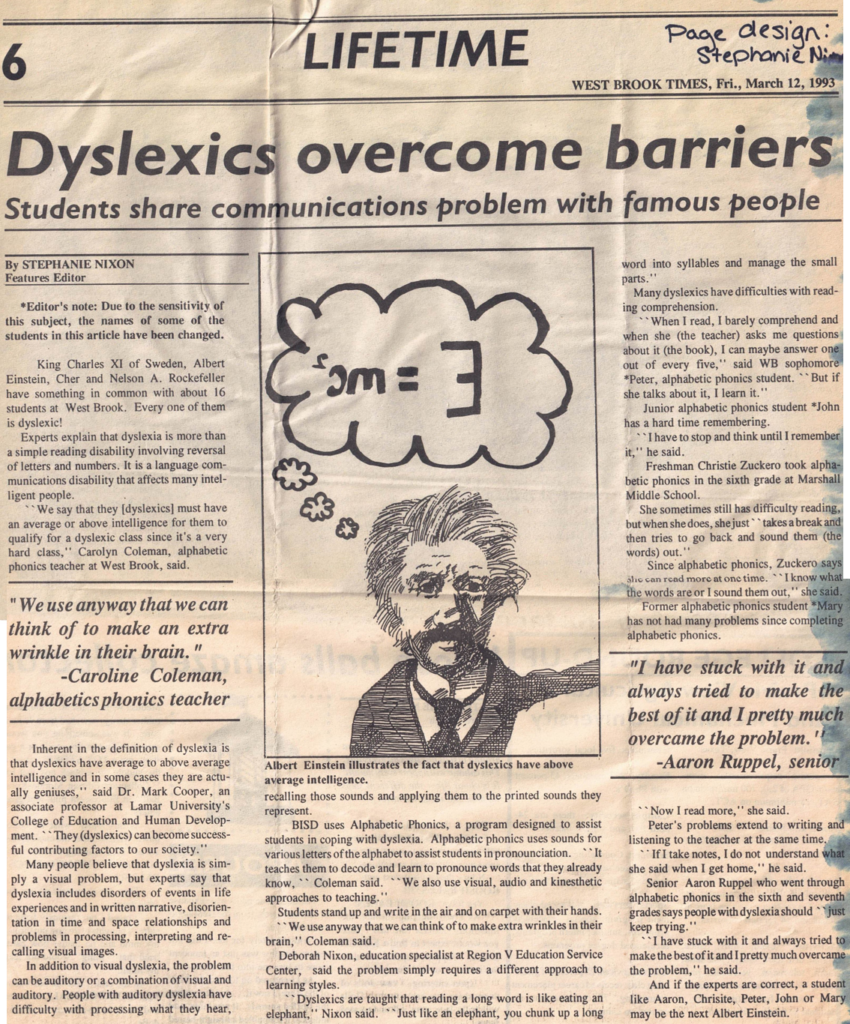
What is disparity? “A noticeable and usually significant difference or dissimilarity”. Think income, education, race, and ethnicity.
Individuals with disabilities (including chronic health conditions, chronic diseases) are another group that might experience health disparity, but there is less research on this group. Krahn, Walker, and Correa-De-Araujo (2014) discuss the history and definitions of disability.
Disparities across income, education, race, and ethnicity
Hoagland, Yu, and Horny (2024) examined the association between patient demographics and insurance denials for preventive care among a cohort of 1,535,181 privately insured patients seeking preventive care in the US.
What preventive care was considered in this study? Contraceptive administration, breast cancer screening, cholesterol screening, colorectal cancer screening, depression screening, diabetes screening, and wellness visits.
Here is a summary of their findings:
- Patients with low incomes (<$30,000 yearly), high school degree or less, and from minoritized racial and ethnic groups experienced higher rates of claim denials. Most frequently these were noncovered service-diagnosis code pairs and billing errors. (What does this mean? People’s access to basic preventive care is different based on their demographic – or income, education, racial, and ethnic background. This is considered inequity)
- Income: The lowest income group (<$30,000 yearly) had 43% higher odds of any denial than those in the highest income group (benefit denials and billing errors; statistically significant).
- Race and Ethnicity:
- Non-Hispanic black patients had 19% higher odds of denials compared with non-Hispanic white patients
- Hispanic patients had 16% higher odds of denials compared with non-Hispanic white patients
- Asian patients had 54% higher odds of denials compared with non-Hispanic white patients
- Education: Differences were not statistically significant
- Did practitioners resubmit bills (i.e., file the bill again) after denials?
- 32.4% of practitioners resubmitted the claims.
- What amount was unpaid by health insurance? The mean (average) of the unpaid denied claim was $1395. This was left to patients 92.85% of the time and varied by patient income, race, and ethnicity.
- Low-income patients had a higher burden than high-income patients (medians of $412 vs. $365, respectively)
- Non-Hispanic black (median $390), Hispanic (median $464), and Asian (median $522) patients each facing higher costs than non-Hispanic White patients (median $357)
- Smaller differences between less-educated patients (median $384) compared with those who had more education (median $399)
Financial burden for those with disabilities, chronic illness, and chronic disease
Note. I struggled to find research addressing this topic as a disparity, and I know I am not including everything out there. Please share any additional information in the comments or email me.
Below is a summary of what I found.
- Increased chronic health conditions = increased financial burden. The more chronic conditions a person has is associated with an increased financial burden (i.e., increased debt, increased medical debt in collections, and increased out-of-pocket medical costs; Becker, Scott, Moniz, Carlton, & Ayanian, 2022)
- Medical debt = worse population health. Medical debt is associated with worse population health (i.e., more days of poor physical and mental health, loss of years of life, higher mortality rates for all; Han, Hu, & Zheng, 2024)
- If you use health services more, then you’re more likely have a claim denied (Pollitz, Pestaina, Lopes, Wallace, & Lo, 2023)
- Of the “high utilizers” (those with more than 10 provider visits in a year), 27% experienced a denied claim
- Of the “moderate utilizers” (3-10 visits in a year), 21% experienced a denied claim
- Of patients with less than 3 provider visits in a year, only 14% experienced a denied claim
- Consequences of patients whose problems included denied claims (Pollitz, Pestaina, Lopes, Wallace, & Lo, 2023)
- Delays receiving care/treatment (26% for those denied and 13% for those who were not)
- Unable to receive medical care or treatment recommended by the medical provider (24% for those denied and 13% for those who were not)
- Declined health (24% for those denied and 10% for those who were not)
- Paid more for treatment or services than they expected to pay (55% for those denied and 16% for those who were not)
- Pollitz, Pestaina, Lopes, Wallace, & Lo (2023) also noted the following about consumers with denied claims:
- Most patients did not know they had appeal rights
- Most (85%) do not file formal appeals (appeal rights vary based on coverage as do the rules; the process can be complicated)
- Often those who need to appeal the health insurance decisions use a lot of health services, and may be too sick to advocate for themselves. (There are programs, Consumer Assistance Programs, available to help; however, they don’t exist in all states and Congress hasn’t appropriated funds since 2010.)
Han, Hu, Zheng, Shi, and Yabroff (2024) noted that policies increasing access to affordable health care could improve population health.
Keep in mind that most of this information describes associations between chronic conditions, medical visits, and financial burden. This means that the values of the variables (e.g., chronic health conditions and financial burden) provide information about each other. This doesn’t mean that more chronic health conditions causes more financial burden, BUT it does mean we can predict the financial burden more accurately when we know the number of chronic health conditions a person experiences.
But implementing such policies will take time and working with both State and Federal elected officials.
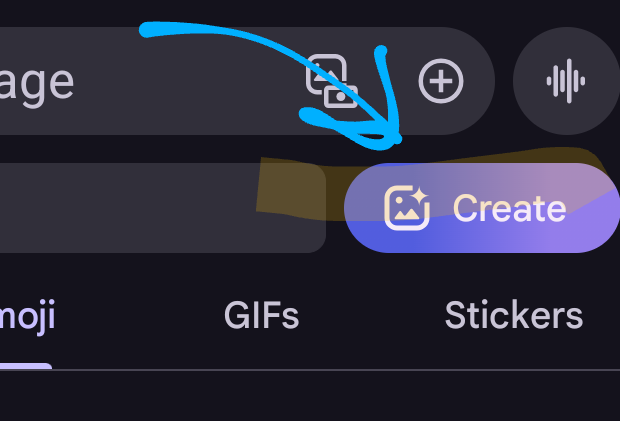
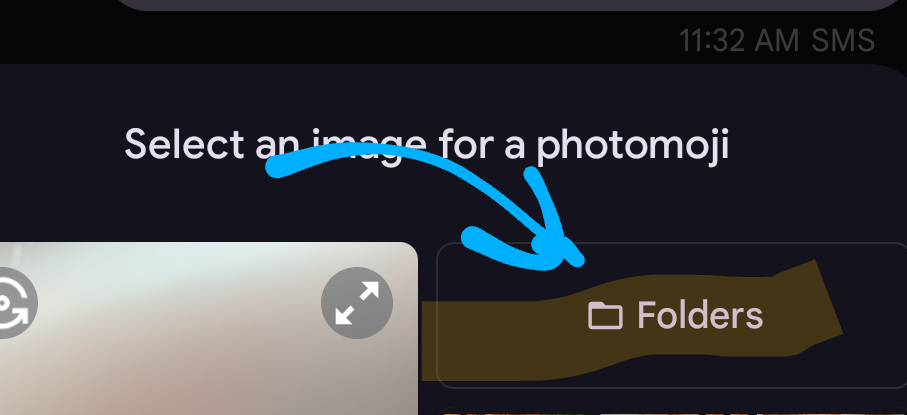
What can you do in the in the meantime?
- Monitor your medical bills
- Know your rights
- Ask questions
- If you don’t understand something your provider puts on a bill OR your insurance company has on the “Explanation of Benefits”, then ask. (You can even ask me)
But please don’t ignore the error. And I understand how exhausting this is. It isn’t easy. It’s frustrating. It is disheartening. It’s overwhelming.
Leave a Reply